Diaphragmatic Excursion on Ultrasound in the ICU

Diaphragmatic excursion refers to the measurement of diaphragmatic movement during the respiratory cycle using ultrasound. In critically ill patients, it is a bedside, non-invasive method to assess diaphragmatic function and to help predict weaning outcomes from mechanical ventilation.
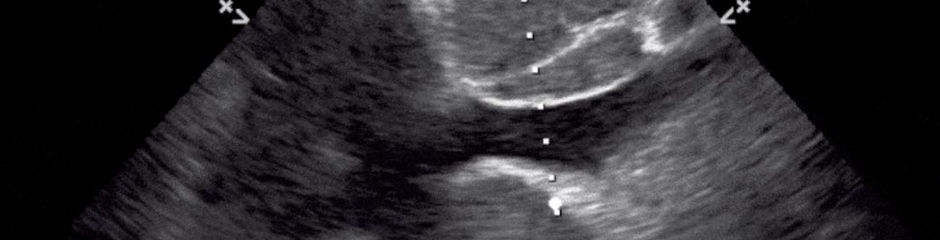
Technique
Probe placement: A low-frequency (2–5 MHz) curvilinear or phased-array transducer is placed in the subcostal or intercostal region.
Window: The liver (right side) or spleen (left side) serves as an acoustic window.
Mode: M-mode is typically used to quantify movement. The ultrasound cursor is placed perpendicular to the diaphragm dome.
Measurement: Excursion is measured as the vertical displacement (in cm) of the diaphragm from end-expiration to end-inspiration.
Normal Values
In healthy individuals:
Spontaneous breathing: 1.5–2.5 cm in women, 1.5–3.0 cm in men.
Deep inspiration: up to 7 cm or more.
In ICU patients: lower values are common, and excursions <1 cm suggest diaphragmatic dysfunction.
Clinical Relevance in ICU
Low excursion (<1 cm): Indicates diaphragmatic weakness or paralysis, often seen in prolonged ventilation, neuromuscular disease, or phrenic nerve injury.
Asymmetry: May suggest unilateral paralysis, pleural effusion, or atelectasis.
Weaning predictor: Reduced excursion is associated with difficulty in weaning from mechanical ventilation. Some studies suggest a cutoff of ~1.2 cm as predictive of weaning failure.
Monitoring: Serial measurements can track recovery or worsening of diaphragmatic function.
Limitations
Operator dependent.
Right side is easier to assess than left (spleen window is smaller, gastric gas interferes).
Accuracy can be affected by patient habitus, subcutaneous emphysema, or poor acoustic window.