Patient-Ventilator Interaction & Asynchrony
- Mazen Kherallah

- Jan 14, 2022
- 4 min read
Updated: Oct 7, 2022

Patient-ventilator asynchrony (PVA) is a mismatch between the patient's demand and the ventilator during a ventilator breath delivery. Patients can demand a breath at a certain time with a specific pressure, volume, or flow. Asynchrony involves the breath initiation (trigger), flow delivery, or breath termination (cycling). PVAs can be easily detected with the visual inspection of the pressure, flow, and volume waveforms on the ventilator display. The intensivist needs to acquire basic knowledge that guides him or her during the detection and management of such interactions.
The incidence of PVA is quite high and ranges from 10% to 85%. It depends on factors related to the patient, the ventilator, or both. The intensivist should be familiar with all types of PVA as the detection and correction of these problems results in a better outcome. PAV has been associated with patient discomfort and dyspnea as well as the increased effort of breathing and worsening of pulmonary gas exchange with hypoxemia or hypercapnia. It can also be associated with diaphragmatic injury, sleep impairment, and the increased use of sedation or neuromuscular blockade. PVA has a potential implication on the recovery process of critically-ill patients and can lead to an increase in the duration of mechanical ventilation, weaning time, length of stay in the ICU, and likelihood of mortality.
The management of PVA may involve simple interventions such as controlling patient pain, anxiety, or fever. A simple modification of the ventilator trigger, flow, or cycling mechanisms may be all one needs to eliminate PVA. Newer modes of mechanical ventilation, such as adaptive support ventilation (ASV), proportional assist ventilation (PAV), or neurally-adjusted ventilatory assist (NAVA), may reduce PVA and have shown some promise.
The most common PVA types are those related to triggering, such as ineffective effort, auto-triggering, and double triggering. Ineffective triggering may occur as a result of ventilator factors such as an inappropriate sensitivity setting (low sensitivity), the malfunction of the sensitivity mechanism, or a prolonged inspiratory time setting. These problems can be corrected by adjusting the sensitivity setting, switching to flow trigger (flow is more sensitive than pressure), or decreasing inspiratory time on the ventilator. Patient factors may contribute to ineffective triggering such as respiratory muscle weakness, decreased neural drive, or dynamic hyperinflation (auto-PEEP). In these cases, the reduction or discontinuation of neural drive depressants, sedation, or NMBA may improve respiratory muscle weakness or neural drive. The addition of extrinsic PEEP (usually at a value less than the auto PEEP) may be effective in cases of dynamic hyperinflation syndrome.
Double triggering on the ventilator occurs when inspiratory time is set too short relative to the neural inspiratory time or when the tidal volume on volume-controlled ventilation (VCV) is set too low. Increasing inspiratory time or increasing sedation (± NMBA) may be all that is needed to eliminate double triggering.
Auto Triggering occurs when the sensitivity is set too high, when a leak in the system is present, or when there is condensate in the ventilator circuit. Patients may have auto triggering secondary to transmission of pressure or flow oscillations because of cardiac activity. Auto triggering can be corrected with the appropriate setting of the sensitivity, correction of the leak, or removing the condensate.
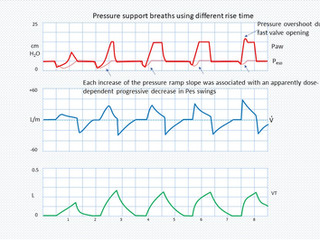
Flow Asynchrony can occur when the ventilator flow is insufficient or excessive in comparison to the patient's need. If the flow is set at a low level in VCV, or the patient's demand is high due to anxiety, fever, or pain, there will be a mismatch between the ventilator flow and the patient's demand. It may manifest clinically with the use of the respiratory accessory muscles, and it will show with a scalloping on the pressure over time curve in VCV. In pressure-controlled mode (or in pressure-support mode), the patient is free to decide his or her inspired flow, but the rise time determines how fast the flow will be. If the rise time is set too slow, the patient may show signs of air hunger clinically. Flow asynchrony can be corrected by increasing the flow in VCV or switching to PCV with a free flow, or by shortening the rise time in PCV or PSV.
Excessive flow may occur if the flow is set too high in VCV or the pressure is too high in PCV or PSV. It can also occur if the rise time is set too short in PCV or PSV. Adjustment of the flow, pressure, or rise time to the appropriate level eliminates the problem.
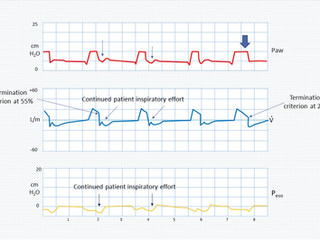
Cycling Asynchrony occurs when the patient terminates their inspiration at a different time than the ventilator. Early cycling is the termination of the inspiratory breath by the ventilator when the patient has not finished their inspiratory efforts yet. This may lead to trigger the ventilator again, causing double triggering. Delayed cycling is the termination of the ventilator inspiration after the patient's inspiration has ended. In other words, the ventilator delivers a breath with a longer inspiratory time than is desired by the patient; that is, the ventilator inspiratory time is longer than the patient neural inspiratory time. Evidence of the patient's expiratory efforts will be shown at the end of inspiration as the pressure spikes. Both problems can be easily corrected with the adjustment of inspiratory time in VCV or PCV, or with the modification of the flow termination threshold in PSV.





















Comments