Should We Change the Defibrillation Strategies in Out-of-Hospital Cardiac Arrest?
- Mazen Kherallah

- May 29, 2023
- 3 min read
Annually, North America confronts over 350,000 sudden deaths from out-of-hospital cardiac arrests, nearly a third of which, equating to roughly 100,000, are due to ventricular fibrillation or pulseless ventricular tachycardia. Despite substantial advancements in defibrillation technology, approximately half of these patients may persist in refractory ventricular fibrillation.
This persistent fibrillation typically renders further standard defibrillation attempts unsuccessful unless the defibrillation approach is revised. To thwart this refractory state, antiarrhythmic drugs such as amiodarone and lidocaine are frequently used. These medications have demonstrated utility in preventing refibrillation. However, their definitive impact on improving patient outcomes, such as enhancing survival rates to hospital discharge or preserving neurological function, remains unclear.
New Defibrillation Techniques
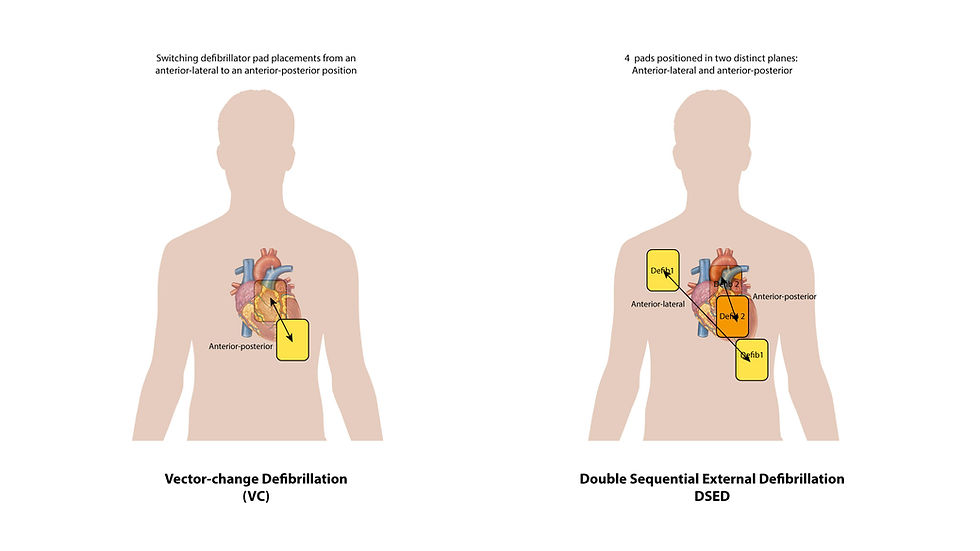
Two new methods allow defibrillation of a section of the ventricle that might be inadequately addressed by the standard anterior-lateral position. The first is Double Sequential External Defibrillation (DSED) involves the use of two defibrillators delivering rapid sequential shocks, with pads positioned in two distinct planes (anterior-lateral and anterior-posterior). A second technique, Vector-change (VC) defibrillation, requires switching defibrillator pad placements from an anterior-lateral to an anterior-posterior position.
Case reports, observational studies, and systematic reviews have discussed the employment of both DSED and VC defibrillation techniques to out-of-hospital cardiac arrest. These reports involved cases or series where DSED was utilized as a final therapeutic resort for patients persisting in refractory ventricular fibrillation. Consequently, these studies may be influenced by resuscitation time bias or by the delayed application of a defibrillation strategy in a subset of patients where a positive outcome was improbable. Cheskes et al. [1] reports in the Journal the results of a large, multiagency, cluster-randomized trial looking at the outcomes associated with the use of these new techniques.
DOSE-VF Trial
It has been proposed that early application of DSED could potentially be linked to higher rates of ventricular fibrillation termination and return of spontaneous circulation in comparison to standard defibrillation. The goal of the Double Sequential External Defibrillation for Refractory Ventricular Fibrillation (DOSE VF) trial was to assess DSED and VC defibrillation relative to standard defibrillation in patients persisting in refractory ventricular fibrillation during out-of-hospital cardiac arrest.
This cluster-randomized trial involved six Canadian paramedic services and utilized a crossover design. Adult patients with refractory ventricular fibrillation were assigned to receive one of three techniques: standard defibrillation, DSED, or VC defibrillation. The primary outcome assessed was survival to hospital discharge, while secondary outcomes included termination of ventricular fibrillation, return of spontaneous circulation, and a good neurologic outcome measured by the modified Rankin scale.
A total of 405 patients were initially enrolled in the study. However, due to the coronavirus disease 2019 pandemic, the trial was prematurely halted by the data and safety monitoring board. Despite this early termination, the results obtained were still insightful.
Among the patients who received DSED, the survival rate to hospital discharge was significantly higher compared to those who received standard defibrillation. The DSED group showed a survival rate of 30.4%, while the standard defibrillation group had a rate of only 13.3%. Similarly, the VC defibrillation group exhibited a higher survival rate of 21.7% compared to the standard group. The relative risks for survival were 2.21 and 1.71, respectively, indicating a substantial improvement with the alternative strategies.
In terms of a good neurologic outcome, DSED was associated with a higher percentage of patients experiencing little to no disability at hospital discharge. The relative risk for a good neurologic outcome with DSED was 2.21, while for VC defibrillation it was 1.48, both compared to standard defibrillation.
Would you consider DSED for refractory ventricular fibrillation?
0%Yes
0%No
0%Awaiting more fresearch
This study highlights the potential benefits of using DSED and VC defibrillation techniques for patients with refractory ventricular fibrillation during out-of-hospital cardiac arrest. Both strategies showed higher survival rates to hospital discharge, with DSED also demonstrating improved neurologic outcomes. These findings suggest that implementing these alternative defibrillation approaches could enhance the overall prognosis and improve patient outcomes in such critical situations.
However, there are some limitations to consider. The trial did not provide information about post-resuscitation care, which could affect the results. Additionally, the trial was terminated early, and the sample size was smaller than originally planned. Combining data from an internal pilot trial with the main trial may have impacted the validity of the results. Moreover, while DSED showed a stronger advantage over standard defibrillation, the confidence intervals for the relative risk estimates of DSED and VC defibrillation overlapped, making it difficult to determine if one strategy is superior.
Conclusion
This trial contributes important effectiveness data supporting the use of DSED and VC defibrillation for refractory ventricular fibrillation. However, further research is needed to better understand the effects of these approaches and to compare them directly. Until then, these extended defibrillation methods should be used with caution and considered when no other treatment options are available.
REFERENCES:
Cheskes S et al. Defibrillation strategies for refractory ventricular fibrillation. N Engl J Med 2022 Nov 6; [e-pub]. (https://doi.org/10.1056/NEJMoa2207304. opens in new tab)





Comments